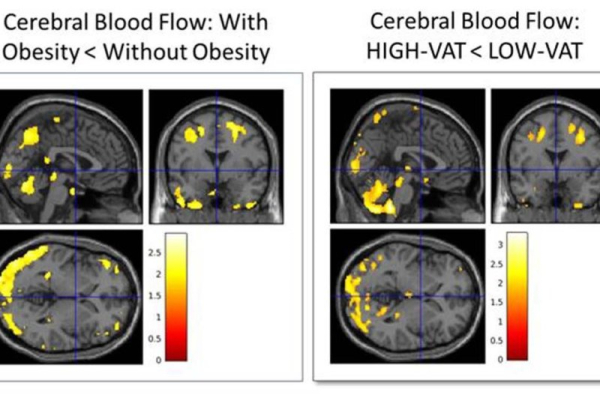
1 of 2 | This comparison of cerebral blood flow in 65 cognitively normal midlife individuals showed that those with obesity and high visceral adipose tissue have reduced blood flow in the temporal and parietal regions of the brain. Image courtesy of the Radiological Society of North America and Dr. Mahsa Dolatshahi
People who are obese and harbor deep belly fat are at higher risk for developing Alzheimer’s disease-specific proteins in the brain up to 20 years before the earliest dementia symptoms, a new study suggests.
The study was to be presented Monday at the annual meeting of the Radiological Society of North America in Chicago. Advertisement
Researchers said the findings emerged from their investigation of Alzheimer’s disease pathology as early as midlife — in the 40s and 50s – when it’s at the initial stages.
They noted that this also is when potential behavioral changes, such as losing weight and reducing fat that lies between abdominal organs, are more effective in preventing or delaying the onset of this neurodegenerative disease.
“Midlife obesity is recognized as the top modifiable risk factor for Alzheimer’s disease in the United States,” lead author Dr. Mahsa Dolatshahi told UPI. Advertisement
However, a healthy diet, physical activity and anti-obesity drugs approved by the Food and Drug Administration can mitigate this risk, said Dolatshahi, a postdoctoral research associate in the Raji Brain Health Imaging Lab at the Mallinckrodt Institute of Radiology within Washington University School of Medicine in St. Louis.
“This points to the importance of lifestyle modifications for better late-life brain health,” she said.
Unlike fat in other areas of the body, deep belly fat is linked to reduced blood flow to the brain and the accumulation of Alzheimer’s disease-specific proteins, known as beta-amyloid and tau.
However, having a higher level of the good cholesterol — high-density lipoprotein — lessens belly fat’s impact on these abnormal proteins in the brain, the researchers noted.
While deep belly fat constitutes a smaller percentage of body fat and is hidden, it does more harm to brain function at levels that are not detectable years before symptoms begin, they said.
According to the Alzheimer’s Association, an estimated 6.9 million Americans ages 65 and older are living with the disease. The association projects that this number could swell to 12.7 million by 2050, unless scientists discover ways to prevent or cure Alzheimer’s.
In this study, researchers followed a total of 80 cognitively normal midlife people with an average age of 49.4 years and 62.5% female. About 58% of participants were obese, and the average body mass index was 32.31. Advertisement
Participants underwent brain positron emission tomography, body MRI and metabolic assessment, as well testing for lipids in the blood. They also consented to MRI scans of the abdomen to measure the volume of fat under the skin and deep hidden fat surrounding the abdominal organs.
The findings showed that higher levels of deep belly fat correlated with increased beta-amyloid, accounting for 77% of the effect of high BMI on accumulation of this protein that is toxic to nerve cells in the brain, the researchers said.
Other experts highlighted that these findings emphasize the significant role that deep belly fat can play in the development of a brain disorder that causes a progressive decline in memory, thinking and reasoning skills.
“This is an interesting and comprehensive imaging-related study that highlights the importance of visceral [deep] fat as a risk factor for Alzheimer’s disease,” said Dr. James Mastrianni, a professor of neurology and director of the Center for Comprehensive Care and Research on Memory Disorders at the University of Chicago Medicine. He was not involved in the study.
“It provides readers with the knowledge that they can control a significant risk factor for Alzheimer’s disease by modifying their lifestyle and diet,” Mastrianni said. Advertisement
The overall message of the study is not surprising, said Dr. Douglas Scharre, a professor of clinical neurology and psychiatry and director of the Center for Cognitive and Memory Disorders at The Ohio State University Wexner Medical Center in Columbus.
“It adds to what we have known previously about the association between cholesterol, obesity and Alzheimer’s disease,” Scharre said.
Nonetheless, an association does not prove causation, said Dr. Kyan Younes, a clinical assistant professor of neurology and neurological sciences at Stanford Medicine in Palo Alto, Calif.
More than half of the study’s participants were obese, so they may have been sicker in general, and other pathways could have contributed to their beta-amyloid and tau accumulation, Younes said.
“It would be interesting to see if these findings hold up in non-obese individuals,” he said.